Reality of my gray matter in black and white
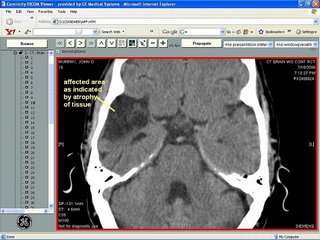
[click on image to increase size;back button to return to blog from larger image]
This morning's posting lands on the "big board" via copy and paste from an email I sent family a few nights ago - please understand and excuse tone or content that might only be appropriate for intra-family correspondence. I'm a little short on time (and grey matter --see image above...no excuse I know, I know).but, I wanted to publish an update regarding recent visits to neurologists - to capture the details of the events as they unfold before the pace of dealing with all the discoveries and implications prohibits a timely and accurate record of events at this phase of my recovery.
I had mixed feelings about reporting discouraging news so soon after the celebration of such dramatic and positive news about my acheivements in last weekend's Heart Walk .But, here's a "healthy spin" on the juxtaposition of last week's great signs of my progress with this week's unfortunate reminder of the gravity of my situation: A "reminder" of the severity of my physical condition only serves to underscore two revelations that I want to make sure are duly noted:
- that my ability to successfully run(jog) a 5K and execute an online fundraising campaign that raised a remarkable $10K shows that I can and hopefully will contine to rise above the physical and cognitive challenges from the stroke I suffered just one year ago.
- that my efforts in documenting my recovery in email and more recently on his blog has been more than just a convenient distraction to keep my mind off the stark reality of my misfortune I'm seeing the potential to alleviate the suffering others might confront from my same or similar twist of fate - i've been touched and amazed by the feedback I've received from dozens of visitors to this site . It is has been surprising to discover just how many people have a grandmother, parent, friend or friend of a sibling, co-worker... struggling with recovery from stroke.
For context (always helpful): Had second visit last week with a new neurologist from whom I have sought a "second opinion" out of frustration over lack of clarity about diagnosis and prognosis for treatment for spasticity (persistent pain and cramping on my affected left side leaving me with sciatica like symptons) -- after 8 months with no improvement and significant negative side effects from oral baclofen therapy. As you might imagine, session w/ this new doctor covered a fair amount of ground and under my present circumstances I’m still processing all of the data (intellectually and emotionally) but the bottom line boils down to about 3 points:
- Images from CT Scans from various phases all confirm hypothesis that issue with spasticity is -as expected- a result of injury indicated in Basal Ganglia (area of brain that sends and receives signal between brain and spine for motor control.
- His view of the nature and extent of injury, based on images he has now seen--as well as my limited progress to date with oral baclofen therapy-- is such that I should not expect improvement along the lines I have enjoyed with recovery of motor control of left leg, arm, and hand. He has repeatedly told me that the best I can expect is 5-15% reduction of intensity of problem and that almost all mainstream oral therapies (like Baclofen and zanaflex) will have the side effects I’m experiencing, as they all impact the central nervous system in a fairly indiscriminate way. This is not encouraging news.... The only alternatives he suggested are from a small handful of other drugs that regulate neurotransmitters – same approach of treatment with slightly different mechanism – he has prescribed one called Lamictal which is used for treatment of bi-polar disorder and (interestingly enough) as an anti-seizure therapy for certain forms of seizures and epilepsy – so this might eventually replace the drug Kepra I’ve been taking twice daily. Given the unfavorable trade-off between the minimal relief and significant side-effects of the conventional oral drug therapies, the second neurologist continues to feel that I am a prime candidate for the baclofen pump - - Ths only raises my suspicions about his enthusiasm for and sincerity in pursuing all other possible oral therapies – this is where I think my current neurologist 's advice will be most valuable. Although I’m still skeptical about the necessity of the Baclofen pump I do see merit in pursuing the epidural baclofen for both diagnostic and therapeutic reasons - so we’ve scheduled that procedure for this Wednesday.My cuurent neurologist agrees that the trial will be a valuable diagnostic tool for a definitive test to assess the efficacy of Baclofen for treating my case of spasticity-- if I don't have a significant positive response to an epidural administration, we can eliminate baclofen from list of alternatives for oral therapies and move on with others asap. He's prescibing a med call Dantraline which we'll start immediately after the baclofen trial on wednesday - assuming the trial will either prove that baclofen is not a viable therapy for my case or that I'll want to try another (potentially effective with less debilitating side-effects) oral therapy option before even considering a therapy as invasive as an intrathecal baclofen pump .
quick update 11/01 : trial produced minimal / inconclusive results.interpretation of results: either a.)baclofen will not be an effective therapy as the source of my spasticity is in basil ganglia not spinal injury - baclofen pump appears to be more effective in instances of spinal injury. or b.) low dose (50 micrograms) administered in trial was not effective due to my high level of tolerence since I have been taking a high oral dose for several month- in which case a second trial with higher dose will be needed to gain definitive finding as to efficacy of intrathecal delivery of baclofen - so I'll start new oral therapy with Dantrolene (dantrium) for a few weeks and consider a second trial of epidural baclofen.
- Only other “significant” issue that arose from review of the images from various stages and sources – was the extent of injury in the right temporal lobe evident in the July 06 scan taken at RI Hospital after my seizure. The radiology reports of October 9, 2005 from Illinois Masonic noted “edema visualized in area of temporal lobe” and reports from other scans on 10/10/05 and 10/11/05 reference “areas of diffusion in right insular cortex …..including smaller focus right occipital lobe suggests acute infarction." – There was also notation of increased edema compared to previous CT in right temporal lobe.
When new neurologist reviewed the July scan he seemed taken aback by size of injury indicated in right lobe – not sure if it was the absolute size or the size relative to my apparent – high level cognitive functioning I’ll have chance to explore the significance of this finding with Dr Hill and Shilpa(speech/congnitive therapist) with whom I will be working again on addressing the cognitive deficits detected in neuropsych test in august. We can certainly share this finding and ask for feedback from the neurophysiologist who has administered tests in February and August. To save you all some time I googled and found site with basic mapping of brain anatomy with function http://www.theuniversityhospital.com/stroke/anatomy.htm
a. “The occipital lobe processes visual information. It is mainly responsible for visual reception and contains association areas that help in the visual recognition of shapes and colors. Damage to this lobe can cause visual deficits.”[This would explain several observations of “performance deficits" noted in testing --as well as problems I’ve experienced at bank machines and navigating menus on some websites and my god damn cell phone;-(
b. The left and right temporal lobes, located around ear level, allow a person to differentiate smells and sounds. They also help in sorting new information and are believed to be responsible for short-term memory. The right lobe is primarily involved in visual memory (i.e., memory for faces and pictures). The left lobe is primarily involved in verbal memory (i.e., memory for words and names).Again these exact issues are evident in testing and in personal experience.
I’ve posted a screen capture of one image from the CT Scan taken in July so you can see the area of injury (I’ve marked and annotated one of the images) so you can locate the “missing grey matter" in question - Several doctors explained that the scans from October show location but would not depict the eventual size or extent of damage as it takes time for the swelling present that soon after the stroke to recede and for brain tissue to atrophy and eventually be displaced by fluid (that’s my interpretation of what I think they said). Hill's remarks on this finding was that he feels that I'm not exhibiting loss of vision field - but that the performance deficit is related more to a problem with visual encoding and processing speed - both of which will be more pronounced in situations that are a.)new/unfamiliar to me or b.)in situations when / where I am multi-tasking.. His other encouraging observation is that because he has observed and read in reports that I am making progress he expects I will continue to see improvement. He'sparticularly impressed and encouraged by findings that I continue to recognize and verbalize to him and family members how and when situations present a challenge and for this reason he expects that I willl be able to learn and apply adaptive techniques to help me manage these challenging situations. Since I'm at a point where I'm considering increasing my hours and scope of responsibilities at work I'm returning to a formal schedule of speech/ cognitive therapy through the day program at St. David's .Primary focus will address deficits in visual encoding and processing speed- with the plan to administer a third round of neuro psych testing to measure progress from results of test in February 06 and August 06, I'll be working with Shilpa with whom I worked previously - which has the obvious benefit of continuity and her knowledge of my history and performance levels with visual encoding and processing speed in context of therapeutic environment.

